How Successful Are Dental Implants?
How Successful Are Dental Implants?
Success rates of dental implants vary, depending on where in the jaw the implants are placed but, in general, dental implants have a success rate of up to 98%. With proper care (see below), implants can last a lifetime.Can Anyone Get Dental Implants?
In most cases, anyone healthy enough to undergo a routine dental extraction or oral surgery can be considered for a dental implant. Patients should have healthy gums and enough bone to hold the implant. They also must be committed to good oral hygiene and regular dental visits. Heavy smokers, people suffering from uncontrolled chronicDoes Insurance Cover the Cost of Dental Implants?
In general, dental implants are not covered by dental insurance at this time. Coverage under your medical plan may be possible, depending on the insurance plan and/or cause of tooth loss. Detailed questions about your individual needs and how they relate to insurance should be discussed with your dentist and your insurance provider.What Is Involved in Getting a Dental Implant?
The first step in the dental implant process is the development of an individualized treatment plan. The plan addresses your specific needs and is prepared by a team of professionals who are specially trained and experienced in oral surgery and restorative dentistry. This team approach provides coordinated care based on the implant option that is best for you.
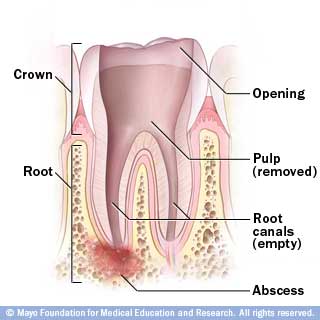
Next, the tooth root implant, which is a small post made of titanium, is placed into the bone socket of the missing tooth. As the jawbone heals, it grows around the implanted metal post, anchoring it securely in the jaw. The healing process can take from 6 to 12 weeks.
Once the implant has bonded to the jawbone, a small connector
Instead of one or more individual crowns, some patients may have attachments placed on the implant that retain and support a removable denture.
Your dentist also will match the color of your new teeth to your natural teeth. Because the implant is secured within the jawbone, the replacement teeth look, feel, and function just like your own natural teeth.